How to Get Relief from Cavity Pain

Key Takeaways:
- Cavities may be caused by one or more of these: enamel erosion from acids, poor oral hygiene, diet, or dry mouth and can lead to pain if untreated.1,2,3,4
- Early cavity pain may feel brief and sharp, triggered by cold, heat or sweets, while advanced decay can cause lingering and radiating discomfort.1,6,7
- Temporary relief options include over-the-counter pain medication, numbing gels, mouth rinses and avoiding extreme temperatures.8,9,10
- Prevention through good oral hygiene, a healthy diet and regular dental visits, is essential.1,3,11,12
How to Help Get Rid of Cavity Pain
Feeling a sharp twinge in your tooth? If you’re dealing with tooth pain, there is a good chance you may have a cavity, and the first thing you want to do is get relief. While cavities can be painful, understanding their causes and knowing how to seek both immediate and long-term relief can make a big difference.
What Is a Cavity?
Dental cavities, also referred to as caries, are permanent damage caused by tooth decay. They can range from small depressions to advanced holes deep in the tooth.1,2
What Can Cause a Cavity?
Multiple factors can contribute to cavities, such as:
- Poor dental hygiene. Not brushing twice daily with fluoride toothpaste, not flossing and skipping regular dental checkups may lead to cavities.1,2
- Diet. Sugary drinks, sweet treats, and starchy foods like bread and cookies can leave a sticky layer on your teeth called plaque. Plaque is made up of bacteria. If you don’t brush it away, these bacteria feed on leftover sugars and starches from food and produce acids. Over time, these acids slowly wear down your tooth enamel, which can lead to cavities. You may be more likely to get cavities if your enamel is softer due to genetics such as hypo-mineralization or a lack of key nutrients like vitamin D and calcium.1,2,3
- Dry mouth. Saliva moistens and breaks down food, washes away food particles from the teeth and gums, and contains important minerals, like calcium and phosphate, that maintain enamel health. Xerostomia, or dry mouth, occurs when the mouth doesn’t produce enough saliva to stay moist.4 Some medications, smoking, dehydration, mouth breathing and other conditions can cause dry mouth.4
What Does a Cavity Look Like?
You can’t always see a cavity. Early decay may appear as white spots, which may be hard to notice, but once a hole forms it can also appear brown or black.1 As tooth decay progresses, these indentations deepen and become more discolored.1
What Causes Cavity Pain?
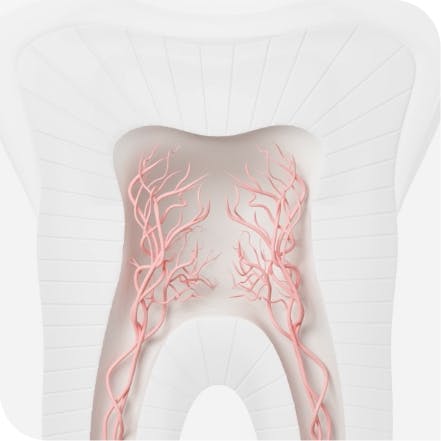
- Exposed dentinal tubules. Tiny channels inside the tooth connecting the inside of the pulp near the nerve to the enamel are called dentinal tubules.5 Exposed dental tubules can result in dentin hypersensitivity, which could seem like cavity pain as it results in sharp pain triggered by cold and sweets, and lasts less than two seconds.5
- Pulpitis. When cavities progress, bacteria can reach the pulp at the center of the tooth where nerves lie, resulting in pulpitis.5,6 This pulp becomes inflamed as a result and causes more intense pain as it advances.5,6
- Abscess. If tooth decay remains untreated, it can develop into a dental abscess, a buildup of pus caused by bacterial infection.7 This pain is severe, often radiating to the gums and requires a visit to your dentist as soon as possible.7
What Does Cavity Pain Feel Like?
Cavity pain exists on a spectrum. In the early stages of tooth decay, discomfort may appear to be triggered by cold or sweets and lasts less than 2 seconds. When tooth decay becomes deeper, the pain can become more intense, lingering, throbbing or even radiating discomfort.1,5,6 In the most serious cases, you may not feel any pain at all— advanced pulpitis can progress to pulp necrosis, meaning the pulp tissue inside the tooth has died.6
- Regular dental visits. Periodic check-ups and professional cleanings are crucial.
- Good oral hygiene. Brushing and flossing regularly can prevent cavities. Using fluoride products can further enhance protection.
- Dietary choices. Reducing the intake of sugary and starchy foods can help. Consuming vegetables is a healthier option.
How to Stop Cavity Pain Fast
Cavity pain can strike unexpectedly, and when it does, it can be both sudden and intense. Whether you’re between dental visits or waiting for a scheduled appointment, immediate pain relief is critical. While it's essential to visit a dental professional for persistent discomfort, several remedies and over-the-counter solutions may temporarily relieve cavity pain.
1. Consult a Dentist
While not an instant fix, visiting a dental professional is the most reliable way to address cavity pain. They can thoroughly assess and recommend appropriate treatment.
2. Take Over-the-Counter Oral Analgesics or Topical Pain Relief
- NSAIDs: Drugs like ibuprofen and naproxen can reduce inflammation. They can be taken alone or combined with acetaminophen.8
- Mouth rinses. Use a mouth rinse that offers temporary immediate relief, like those containing local anesthetics like lidocaine or benzocaine.9
- Numbing gels. Over-the-counter numbing gels can be directly applied to the affected tooth.10
Long-Term Cavity Pain Relief Solutions
Immediate remedies only provide temporary cavity pain relief; they are not a lasting solution. Persistent pain or untreated cavities can lead to severe dental issues. These long-term treatments can address the root cause and prevent further oral disease:
- Fillings. The dentist will remove the decayed portion of the tooth and restore it with a filling.
- Crowns. If the tooth's structure is significantly damaged, a crown, a tooth-shaped cap placed over an existing tooth or implant, may be required.11
- Root canals. In cases of pulpitis, a root canal may be necessary to remove the inflamed pulp, thoroughly clean the inside of the tooth and then fill it back and seal it to restore function.12
How to Prevent Cavity Pain
Prevention is always better than cure, especially with dental health. Taking proactive steps to maintain a healthy oral environment can reduce the risk of developing cavities in the first place. You can effectively help keep painful cavities at bay with these habits:
- Regular dental visits. Periodic check-ups and professional cleanings are a must.
- Good oral hygiene. Brushing twice daily with a sensitive-friendly fluoride toothpaste like Sensodyne and flossing at least once daily can help prevent cavities.1
- Dietary choices. Reducing the intake of sugary and starchy foods can help. A nutritious diet high in vegetables, fruits, and healthy protein sources is a healthier option.1
- Drink water. Drinking water washes the acidic PH level away. Have a glass of water between meals.1
With these tips, you can hopefully find temporary pain relief. Remember, the information provided here is general advice. Always consult your dentist for personalized recommendations and treatments.